
S11
A n a i s d o I HM T
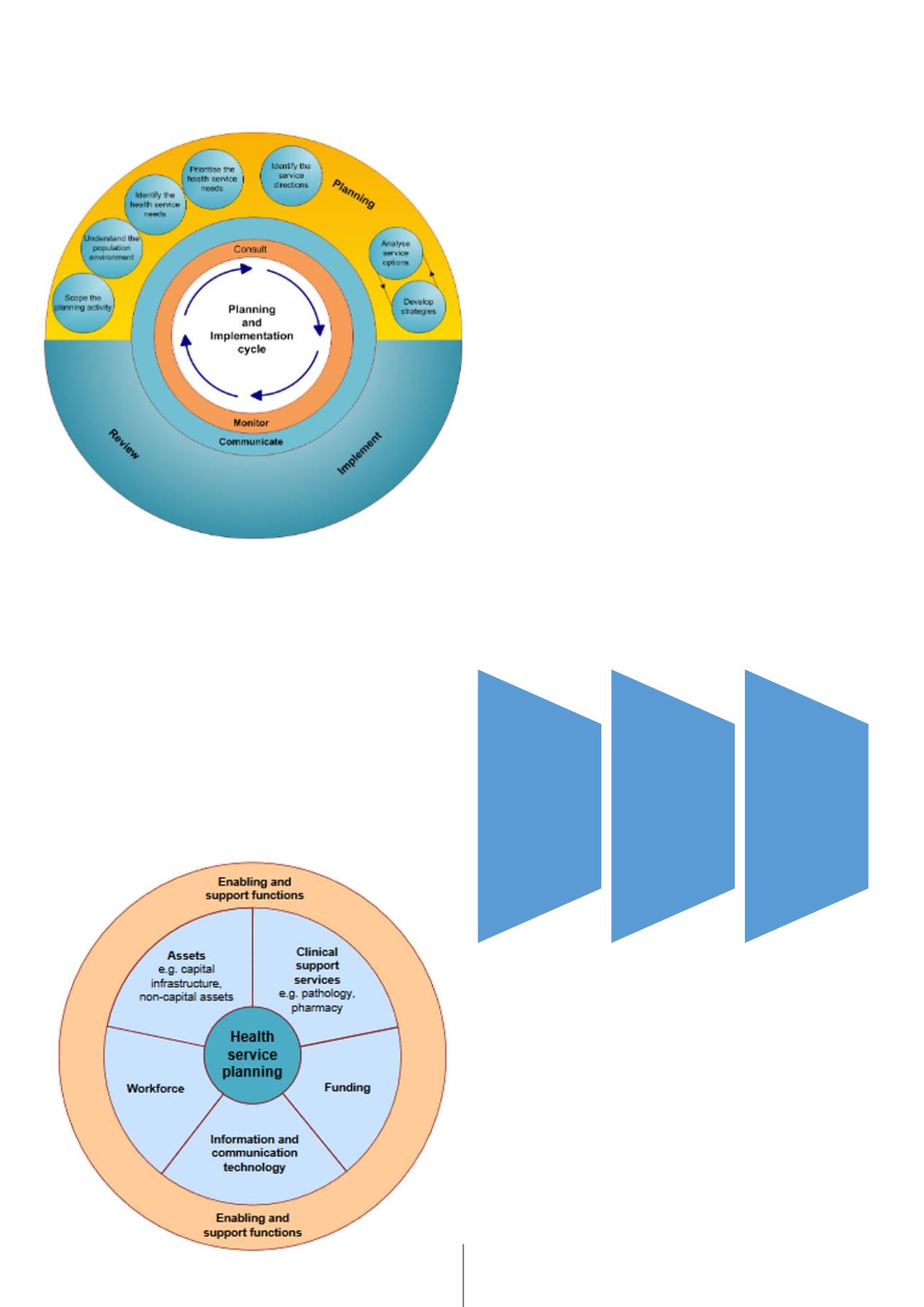
Figure 2 shows some of the elements that go into the
planning part of the cycle, locating the plans firmly
in a wider analysis of the population and their health
needs. Each of these elements is described in the plan-
ning guide. Figure 3 below identifies the different ele-
ments of the supporting and enabling functions from
the clinical support services to funding and the work-
force which need to planned for and aligned with the
wider plan. The whole process represented by these
two figures is a complex and logical approach to plan-
ning which attempts to make sure that every relevant
factor is considered before the plan is complete.
Since 2012 England has adopted has adopted a far sim-
pler and more market-driven approach to planning. It
is summarised in a rather simplified version in the fol-
lowing paragraph and Figure 4.
At the national level the Government agrees an annual
mandate with NHS England which sets out the Govern-
ments objectives and funding for the year. [6] As part
of this, NHS England and all health bodies are required
to work within the framework of existing national
policies on everything from professional regulation to
accountability and patient safety. NHS England is an
arms-length public body accountable to Parliament
(rather than Government) and is responsible for ar-
ranging the provision of health services in England. It
in turn allocates funding and provides guidance to the
purchasers
of health services, which are mainly family
doctor’s practices, to
commission
services for their local
populations.These commissioners contract “any willing
provider” from the public, private or voluntary sectors
to deliver services. [7]
The English model is very different from the Queens-
land one. It is focussed on delivering objectives rather
than on determining how this should be done and, in
the original intention of the Bill that introduced it, on
promoting competition between providers. There was
an underlying assumption that regulation and the invisi-
ble hand of the market will provide better solutions and
services though competition than planning could ever
do.This model means that planning in the Queensland
sense is almost entirely the responsibility of the 221 lo-
cal commissioners or Clinical Commissioning Groups
which on average serve populations of about 220,000
people.
A more extreme version of this model can be seen in
the US where Government regulates but does not pro-
vide a
mandate
, there is no equivalent of NHS England
Fig. 2:
The Queensland Planning and Implementation Cycle [4]
Fig. 3:
Queensland – the Enabling and Supporting Functions [5]
Fig. 4:
Simplified version of how services are commissioned in England
Anais of the Instituto de Higiene e Medicina Tropical
January 1, 2017
NIGEL CRISP
4
Figure 2 shows some of the elements that go into the planning part of the cycle, locating the
plans firmly in a wider analysis of the population and their health needs. Each of these
elements is describe in the planning guide. Figure 3 below identifies the different elements
of the supporting and enabling functions fro the clinical support s rvices to funding and the
workforce which need to planned for and aligned with the wider plan. The whole process
represented by these two figures is a complex and logical approach to planning which
attempts to make sure that every relevant factor is considered before the plan is complete.
Figure 3: Queensland – the Enabling and Supporting Functions
v
Anais of the Instit to de Higiene e Medici a Tropical
January 1, 2017
Since 2012 England has adopted has adopted a far simpler and more market-driven approach
Anais of the Instituto de Higiene e Medicina Tropical
January 1, 2017
NIGEL CRISP
6
Figure 4: Simplified version of how services are commissioned in England
The English model is very different from the Queensland one. It is focussed on delivering
objectives rather than on determining how this should be done and, in the original intention of
the Bill that introduced it, on promoting competition between providers. There was an
underlying assumption that regulation and the invisible ha d of the market will p ovide better
solutions and services though competition than planning could ever do. This model means
that planning in the Queensland sense is almost entirely the responsibility of the 221 local
commissioners or Clinical Commissioning Groups which on average serve populations of
about 220,000 people.
A more extreme ersion of this model can be seen i the US where Government regulates but
does not provide a
mandate
, there is no equivalent of NHS England and service planning is
undertaken by insurers which generally aren’t linked to a specific geographical area and have
no responsibility for population health.
The UK model has already changed considerably from the original intention of the Bill. In
practice co petition is larg ly managed so as to preven major disruptio s to local services –
and unnecessary duplications of service - and most recently to introduce a level of planning at
a higher level in the system. The system as introduced meant that, with the exception of
highly specialised services which are commissioned nationally, no one had responsibility for
planning across the local commissioning boundaries. This meant that many important
Government
• determines overall
policies and
funding
• agrees
mandate
with NHS England
covering
objectives and
funding
NHS England
• responsible for
securing services
in all parts of
country
• funds and
provides guidance
for local
commissioners
Commissioners
• responsible for
securing services
for local
population
• contracts with
"any willing
provider"


















